In February 2016, I had a recurrence in my liver and lung, and spent much of that year on chemotherapy. In February 2018, I had another recurrence, again in my liver and lung, and spent much of that year having surgeries. As such, it should come as no surprise that in February 2020, I’ve had another recurrence…
The discovery of this, my fourth, recurrence started on Thursday 30th January with a CT scan and an MRI scan. The hospital managed to book both scans into the same day, which was much appreciated and saved me a trip to the hospital. There then followed the traditional two weeks, or so, of slowly increasing tension and stress known as Scanxiety.
Until, on Wednesday 12th February 2020, I had my appointment with the oncologist. The appointment was with a new oncologist, because the one I’d been with until then had moved on to bigger and better things. This, for me, was something of a disappointment, because I’d formed a working relationship with the previous oncologist. She was also very good. February 2020 would be the start of a new era.
Our relationship, though, was a complicated one. I liked knowing where I stood, but she didn’t like giving specifics in her answers. So I asked carefully phrased, ‘hypothetical’ questions. And she responded with carefully phrased ‘hypothetical’ answers…
It was like a code. Or a dance.
Anyway, it worked, and we both left the meetings content in what had transpired.
But I didn’t have that sort of relationship with the new oncologist. In fact, I didn’t have any sort of relationship, as we’d never met. I think that it was fair to say that I was nervous to meet him.
Nerves that weren’t helped by the fact that he was running quite late with his appointments. An hour late, it would eventually transpire. And an hour is a pretty healthy chuck of time to drag by, when you’re already up to your ears with scanxiety. When we finally got called through, it quickly became clear that the reason that he was running late was that he was having one of those days.
The kind of day when all you seem to be doing is giving your patients bad news.
His ‘bad news’ streak certainly didn’t come to an end during his appointment with me.
Fortunately, I’m an old hand, when it comes to receiving bad news.
He was also reasonably forthcoming with the juicy details, which made my life easier. That said, he started with, “Well, the CT scan was clear.”…
Yeah, like that was going to fool anyone!
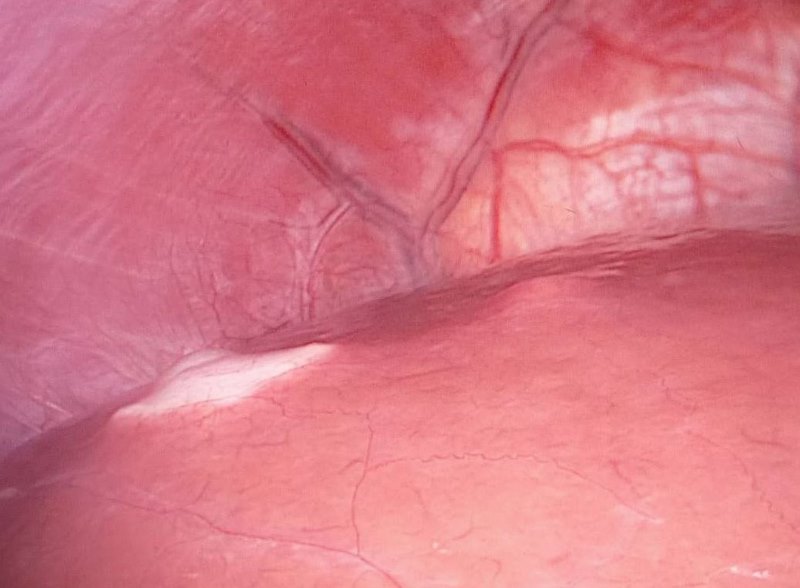
The CT scan, which checks me from neck to nuts, never seems to show up anything that appears in my liver. In the past, the reason given for this was my weight. But I was much lighter, this time around. Anyway, my lead-lined liver is the reason that I’m also given an MRI scan, just of the liver. The MRI scan showed a ‘small’ tumour had popped up in ‘lobe 2’.
And it’s usually at this point that the battle for clarity of information begins. Historically, I would ask something like, “What constitutes ‘small’?” And would be met with a vague answer, necessitating the start of the coded dance.
Not with this guy, though. He broke out the images of the scan and pointed out the tumour. “It’s at 35mm,” he said.
“And that’s classed as small…?!” I asked, somewhat incredulously.
“Oh, yes.” He replied. And then went on to explain that it wasn’t the size that was the issue, it was the location.

M’eh! I’ve had bigger…
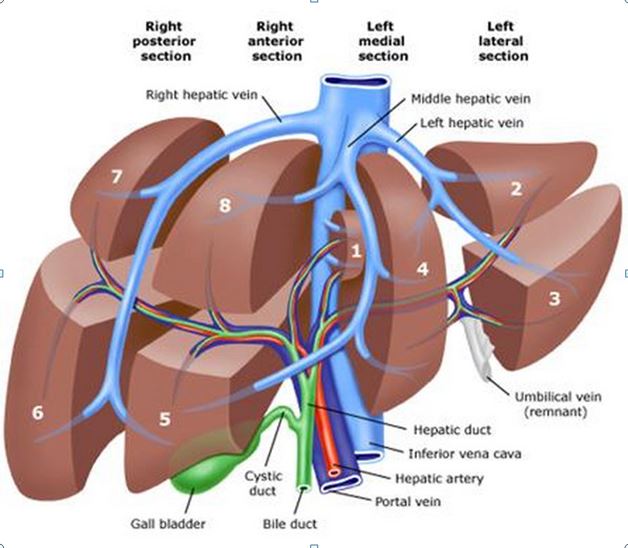
The tumour is situated next to a reasonably sized blood vessel in lobe 2 (see image, below). And the MRI scan wasn’t clear enough to tell whether said blood vessel is clear of the margins of the tumour (I’m probably not phrasing that correctly, but I’m sure you get my meaning). If it isn’t clear, then things become more complicated.
As I’m sure everyone knows, the liver can regenerate. Which is to say that you can remove great swathes of liver tissue and it’ll just grow back. I’ve always admired that in an internal organ. It can only do this, however, if the surrounding infrastructure remains intact. If the liver tissue doesn’t have a blood supply, it can’t regrow. So, if the blood vessel gets taken with the tumour, none of the tissue downstream of that point can regrow.
In essence, this makes the liver smaller. And a smaller liver means that there is less room for future tumours to set up base. Thus making future recurrences more likely to be near something vital. And, as I’ll get to in a bit, there will be future recurrences.
It has already been explained to me a couple of times before that it’s important to keep as much of the liver intact for as long as possible. Because this, in turn, will allow me to keep going as long as possible. And, to find out what this particular tumour had in mind for the future of my liver, I’d need a PET/CT scan. Which I’ve actually now had.
I had the PET scan on Tuesday 24th February 2020: Shrove Tuesday. Or Pancake Day, if you will. Which is actually today… (at least, it is for me; because this is when I’m writing this bit).
Ceri made pancakes. But I couldn’t have any, because I was out playing hockey. In the hail! Not that I’m actually that big a fan of pancakes (don’t tell anyone). Or playing hockey in the hail, as it turns out (it’s okay to mention this…).
And so the scanxiety begins in earnest.
For me, scanxiety is always based around the uncertainty involved. And this scanxiety is particularly intense because, depending on the PET scan results, there are two entirely different paths open to me.
If the tumour in the liver is operable, I’ll get a call from the Spire Hospital, in Bristol, to go and have a chat about when we should do the surgery. If I don’t, I’ve been given an appointment on 11th March to go into Musgrove Park Hospital, in Taunton, to talk about radiotherapy.
On the one hand, it’d be cool to have a new treatment to write about. On the other hand, radiotherapy isn’t as effective as surgery…
Tough decision.
Not that it’s mine to make. The PET scan will make that for me.
The radiotherapy treatment could well be of the Sterotactic variety. But, as I’m not sure yet, I won’t go into any detail of what SABR or SBRT might involve. I’d hate to ruin the surprise! Besides, it’s February now and who know how far things will have progressed by just the end of 2020?!
All I can do, at this point, is hope that I get a call from Bristol before the 11th. Oh, and wait. I do get to do a lot of, waiting uncertainly for a call, that might or might not come. A call to maybe invite me for surgery at some unspecified date in the future. It’s going to be a loooooong two weeks!
So, getting back to the bit where I said that I was expecting more recurrences. Well, there’s a reason for this expectation; the hospital put me on palliative care back in 2016. As far the hospital is concerned, I’m terminally ill and that won’t change unless a new form of treatment is developed that can cure me.
And the reason that I mention this, is that there can be confusion about what a recurrence actually is. Essentially, a recurrence isn’t a new illness. It’s still all part of the original disease.
I was diagnosed in 2014, and so a figurative battle started between my body and the cancer within it. At the point of diagnosis, the cancer was winning quite comfortably, having been carrying out an unnoticed sneak attack for months, if not years. The chemotherapy and surgery I had during 2014 forced the cancer into retreat. My body won that battle.
But the cancer regrouped and attacked a couple more times. The first time being repelled with surgery and the second, in 2016, by chemotherapy. It was with this second lot of chemotherapy that the hospital accepted that my war was lost. Thankfully, no one explained this to my body, which fought on valiantly.
And, so, the cancer was forced into retreat again. Until 2018, when it took another crack. This time, as before, it was knocked back by surgery, and retreated once more to consider its options.
Which brings us to February 2020, when the cancer has once again attacked my liver. This time in Lobe 2.
And so the war rages on; into February 2020, and beyond…
My point, here, is that I’ve never ‘beaten’ my cancer. This isn’t another diagnosis of a new cancer. I’ve only had cancer the once, and it’s been coming at me in waves since 2014. It’s all the same illness.
And I, for one, wasn’t expecting things to progress like this.
My understanding, until really quite recently, was that I had a different path to travel.
My original, primary, tumour was in my large intestine. By the time it was found, it had grown so large that it had become able to send out metastases. In essence, when a tumour reaches a certain point of size and complexity, bits of it can break off and reattach elsewhere in the body. Once in a new location, the little bit of the original can grow and become a secondary tumour.
Now what I’d thought was that these secondary tumours had to go through the same process as the primary. I thought that each secondary tumour would have to grow to reach a specific size and complexity before it, too, could start breaking apart and having little metastases of its own. Tertiary tumours, I suppose.
Except that, ‘tertiary tumours’ isn’t a thing.
Because, and this is the bit that got me, all secondary tumours are already at the necessary size and complexity to create metastases, no matter how small they are.
Which means that the idea that I’d been working to, for a number of years, was simply wrong.
I’d assumed that the primary tumour could only have released a finite number of metastases before it was cut out. All I had to do was stay alive long enough for all of these metastases to be discovered and removed, and then I was done. And, because I was having such regular scans, none of these secondary metastases would ever reach a sufficient size and/or complexity to make metastases of their own.
It was a simply, workable theory, with only one slight flaw: it was utterly wrong.
As it turns out, all metastases can produce more metastases at the drop of a hat.

To further complicate matters, chemotherapy works in much the same way as antibiotic resistance. When you use antibiotics on bacteria, if any of the bacteria survive the dose, they are then immune to that type of antibiotic. Well, the same is true of cancer cells and chemotherapy. Any cancer cells that survive a dose of chemotherapy are not affected by that type of chemotherapy in the future.
And I’ve had both of the recognised types of chemotherapy for bowel cancer. Which means that all of the tumours that have popped up since 2016 are descended from cancer cells which have survived both types of chemotherapy. In my case, chemotherapy has been very much relegated to a last resort. The longer I go before the next dose, the greater the chance that the cancer cells in my body might have evolved from their utterly-immune ancestors. In which case, the chemotherapy will have some genuine impact.
Of course, more treatments are being developed all the time. As was recently pointed out to me: when I was first diagnosed, HIV/AIDS was perceived as a death sentence. Yet, now, there are antiretroviral drugs that allow AIDS patients to live long, healthy lives. If it can happen for HIV/AIDS, it can happen for cancer. Maybe not in February, but there’s plenty of 2020 to go yet…
In fact, just last month, in Cardiff University, a new discovery was made. One that has the potential to act as a universal cancer therapy. Possibly even the holy grail of a cure for all cancers. I accept that this is pretty unlikely. It is, however, being actively researched. And, if all goes well, treatments could be available within a few years.
And, if that doesn’t sound like hope, then I don’t know what does!
But, if you think I’m going to spend my time researching this ‘potential cure’, and writing up a post about it, well… you’re absolutely right!
You can expect something in the next couple of weeks.
By which time, I should have a better understanding of how this recurrence is going to be dealt with. Something I will talk about in the March 2020 update.
February 2020 marks the start of the next chapter of my illness. The main thing I have to do between now and hearing what my next treatment will be is, not eat too much. Although, in reality, that ship has sailed. So, I figured, what the Hell, I might as well make the most of it. Which is why we’re off to a Kaspa’s this weekend…
Did you know that there’s a restaurant chain, just for desserts? I certainly didn’t, until Ceri mentioned it a couple of weeks ago. After that, a visit was inevitable!

Nom Nom Nom.

6 thoughts on “Progress Update for February 2020”
Thanks for taking the time to post this. The information is quite eye opening! My husband had a tumor removed from his cecum 5 years ago and has never had another scan since then. The Doctors are more concerned with his PSA count, go figure. Probably because we have crappy insurance (government provided)! Hang in there and just try to make the most of every day. Hug those teenagers and your wife often. Looking forward to hearing more about the possible cancer cure you are researching.
Hi Cindy,
It’s nice to hear from you again.
If your husband’s tumour was successfully removed, in a nice, straightforward surgery, particularly if it was caught early, there’s a good chance they know they got it all. Which means your husband shouldn’t need any more scans. When my dad’s (colon) tumour was removed, they basically washed their hands of him. They knew they’d done a good job and, more or less, left him to his own devices. This was more than 20 years ago, and he’s still going strong.
I’m dragging one of my daughters around the Royal Mint (which makes the UK coins), next week. If that doesn’t count as quality time, I don’t know what does!
Actually, now I think about it, the Royal Mint is just outside Cardiff, which houses the University that is doing the research on the cancer cure. And the reason we’re there at all is because I’m taking my daughter to interview for a place on their Pharmacy course. It’s a small world, sometimes.
Maybe I can get some photos for the post about the cure…
Anyway, heath and happiness to you and your husband.
All the best,
Paul
Hi ,interesting news especially the change in oncologist,do you think you’re new oncologist will have a fresh approach ,in my friends case his oncologist has been quite flippant of late,almost as if he also is going on to bigger and better things I’m thinking perhaps another opinion may be necessary in my friends case as this specialist keeps apologising for the severity of the treatment offered,due to the side effects experienced by my friend .
Hi Jan,
My previous oncologist understood that I want to tackle my recurrences in the most ‘aggressive’ way possible. Which is to say, surgery every time I can. ‘Aggressive’ is the term that is used by the consultants that I see. I’m not sure that it’s the term that I would choose do describe a preference for surgery, but it’s not up to me. Anyway, both I and my previous oncologist have learned over the years that, for whatever reason, I handle surgeries very well. I heal very quickly and couldn’t care less about scars (which is probably just as well!).
This new oncologist initially started discussing the radiotherapy options. It may turn out to be that this is because he could see the writing on the wall, and the PET scan will show that it’s going to end up being radiotherapy. It could, however, be that he just tends to favour a less ‘aggressive’ approach and will typically recommend non-invasive over invasive treatments. Time will tell.
I have had seen a couple of other oncologists over the years. Typically when my usual one was unexpectedly absent. And it was interesting how they each have their own approach. One I saw (just the once) really approached things from a different angle. She talked about the options for introducing something akin to a radioactive grain of rice into a tumour, and letting it cook from the inside out (it wasn’t actual rice, but a piece of material, about that size).
Anyway, my point is that every oncologist that I’ve seen has had a different way of viewing my case.
With this in mind, it would make sense for your friend to consult with a different oncologist, precisely to get that fresh approach. I think it would be better to get that second opinion, even if your friend ends up getting told exactly the same thing. At least your friend will know he’s getting told the right information. The alternative is not to get the second opinion, until it’s too late to do so, and then forever regretting not doing so. To my mind, in this situation, regrets are best avoided, where possible.
I wish all the best to you and your friend.
Take care,
Paul
We live from our cells but we have not the best cells now. Losing!
Hi there,
Our cells certainly can let us down but cancer survival rates have increased from 25% to 50% in my lifetime.
It might be an uphill battle but I don’t think we’ve lost just yet.
Paul