The only thing that happened to me during March, cancer wise, was a colonoscopy. And because the news is all good, with not even a polyp or biopsy in sight, I thought I’d skip a dedicated ‘March Update’ post. Instead, I’ll look in detail at the process of having a colonoscopy. I have touched on this before, in the run up to being told it’s cancer, but there’s a lot more to having a colonoscopy than you might think. And it’s one of those topics that doesn’t really get discussed much, so I’d like to demystify it…
So, let’s start with what a colonoscopy actually is. Wikipedia defines a colonoscopy as:
‘The endoscopic examination of the large bowel and the distal part of the small bowel with a CCD camera or a fiber optic camera on a flexible tube passed through the anus.‘
This loosely translates as:
‘A flexible tube with a built-in camera, called a colonoscope, will be pushed up your bum until it gets all the way round to your appendix.’
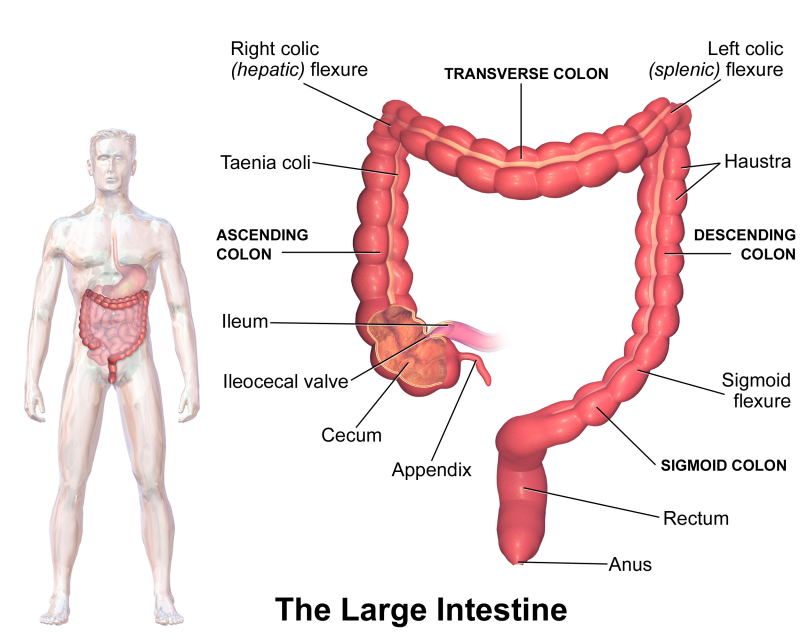
To make this clearer, we need an image of the large bowel (large intestine, or colon):
Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”
I imagine that the next question would be something along the lines of, “Why on Earth would anyone want to have that done!?”
Well, ‘want’ is a strong word.
Colonoscopies are an extremely useful diagnostic tool. Before you get to the stage of actually having a colonoscopy, though, you’ll probably have gone through some other tests first, depending on the urgency of the symptoms you’re showing. The quickest and easiest test, is for a stool sample to be taken for analysis. Assuming that the test reveals issues like, blood in the stool, you could end up having a ‘virtual colonoscopy’.
Having a virtual colonoscopy is just an upmarket way of saying, ‘having a scan’. Either a CT scan or an MRI scan, both have the advantage of being noninvasive. Both have the drawback of not being able to see, or visualise, issues that are smaller than 5mm. If the virtual colonoscopy can’t get to the bottom of the problem, perhaps a sigmoidoscopy can…
A sigmoidoscopy is a toned down version of a colonoscopy. The main difference is the extent of the examination. The sigmoidoscopy is classed as ‘minimally invasive’ because it just takes a peak around the corner, so to speak. That said, typically the preparation for a sigmoidoscopy is the same as for a colonoscopy, which I’ll be covering in detail, shortly. If, as was my case, the sigmoidoscopy still can’t identify the source of your symptoms, then there’s nothing left for it but the colonoscopy.
The beauty of a colonoscopy, from a diagnostic perspective, it that it allows a full visual examination of the colon. Additionally, tools built into the colonoscope allow the operator to take tissue biopsies for analysis. It even allows the removal of polyps, which can then be examined to see if they’re precancerous. As such, colonoscopies are essential tools in the diagnosis of inflammatory bowel disease. And bowel cancer (colon or colorectal cancer).
But there’s far more to having a colonoscopy than the physical procedure. A colonoscopy must be prepared for, and this process usually starts some weeks in advance.
For reasons I will come on to, sedation is offered with colonoscopies. This means that the hospital will have to do a pre-assessment interview to ensure you’re aware of what’s involved and healthy enough to move forward. In times gone past, this would involve a trip to the hospital and a sit down chat with a nurse. More recently, this process is done over the phone. Places will differ in their processes but you can expect to talk to someone at some point.

Assuming the chat is okay, there is a strong likelihood that a blood test will be required. The last time I had a colonoscopy, which was a couple of weeks ago, I was required to have a blood sample taken to check my kidney function. This is because you’ll have to take some seriously powerful laxatives before the procedure. This can leave you dehydrated and with an electrolyte imbalance. If your kidneys are unlikely to be able to cope with this, it’s better to know in advance.
If your kidneys are good, you can progress. You’ll be given your laxatives, mine arrived by post. With the drugs will come a set of instructions about the foods you’re allowed to eat in the run up to the colonoscopy procedure.
Despite the fact that you’ll literally be emptied from top to bottom, it’s important that nothing gets left behind. To this end, you need to follow a ‘low-residue’ diet in the days leading up to the procedure. The ‘residue’ that you mustn’t leave behind, and therefore mustn’t eat, comes in the form of dietary fibre.
On a side note, writing about the eating restrictions relating to the low residue has nudged a memory. One of the common things that you hear from vegetarians and vegans is that meat gets stuck in your bowel. In actual fact, the only thing that the hospital was worried about being left in the bowel, was plant based residue. Completely irrelevant, but vaguely interesting…
Anyway, I started my low residue diet about four days before my procedure. The instructions said to start three days before but, because there’s also a period of fasting, I wasn’t sure if it meant three days before the fasting, or the procedure. So I went three days before the fasting, to be on the safe side.
The guidance I got from the hospital about what I could and couldn’t eat, boiled down to this:
| Food Type | Okay to Eat | DO NOT EAT |
| Cereal Products | White bread, noodles & pasta | Wholemeal bread, noodles & pasta |
| Breakfast Cereals | Rice Krispies, Frosties, etc | Porridge, Muesli, Branflakes, etc |
| Dairy Products | Eggs (not fried), any low fat dairy | Fried eggs, cream, full fat dairy |
| Meat & Poultry | Any lean meat or poultry | Any fried, fatty or processed meats |
| Fish | Any white fish, grilled or baked | Oily fish and any fried fish |
| Vegetarian Foods | Tofu, Quorn, Soya | Vegetarian ready and processed meals |
| Fruit & Vegetables | Boiled potatoes, clear fruit juice | Everything else… |
| Nuts, Beans & Pulses | None! | Any nuts, beans, pulses or seeds |
| Soups & Drinks | Soup with no bits | Creamy, fatty drinks or soups |
| Biscuits & Cakes | White flour cakes and biscuits | Cakes and biscuits with fruit or nuts |
| Puddings & Desserts | Jellies, meringues, custards, etc | Anything fatty, creamy or fruity |
| Confectionary | Boiled sweets, a bit of chocolate | Anything with fruit or nuts |
| Preserves | Seedless jams, honey, syrup, treacle | Whole fruit jams, etc; chutneys, etc |
| Miscellaneous | Low fat dressings |
Basically, avoid anything with fruit, veg, nuts, fibre and excess fat.
Normally, I love the low residue diet. It’s the perfect excuse to binge eat cakes and biscuits, safe in the knowledge it’s all going to get flushed out in a couple of days anyway. I know it doesn’t actually work like that, and I’ll have taken on all those calories, really; but denial isn’t just a river in Egypt.
This time, however, I’m in the middle of a rather effective diet. I’m been steadily losing weight since Christmas and the low residue diet was going to be a major problem, because my diet is based around two bowls of porridge a day. Porridge to which I add dried fruit. Both of which are banned on the low residue diet.
The reason my porridge based diet has been working for me is that the porridge keeps me feeling full. Which means I’m not constantly thinking about food and being tempted to break my diet every 10 minutes. I did a bit of research and found that protein is also known to keep you feeling full. So I switched my two porridge meals for scrambled eggs on toast. The eggs weren’t as effective as keeping the hunger at bay as the porridge had been, but they worked for the three days.
However, one significant difference between a porridge based diet and an egg based diet is the constipation. Protein heavy diets are famed for the constipation they cause. But I figured that I’d be taking the mother lode of laxatives, the day after I finished three days of egg-based eating; that would sort everything out. This turned out to be an unwise assumption…
After the low residue diet comes the fast.
At what point you start your fast will depend on the time of your procedure. If you’ll be having your colonoscopy in the morning, you’ll need to fast for the entirety of the previous day. I was having my colonoscopy in the afternoon, which meant that I was allowed a light meal at around 1pm on the day before. In essence, you’ll need to fast for 24 hours before having your colonoscopy.
The time of your procedure also dictates the time you take your laxatives, at the end of your fast. There are two doses of laxatives to take.
Also the pint of fluid that you’re supposed to drink alongside the laxative. It’s probably supposed to be a clear fluid, but I needed something with flavour.
If you’re having your colonoscopy in the morning, you’ll take one dose of laxatives the afternoon before the procedure. You’ll take the second dose that same evening. This means that you’ll be completely done by bed time. You can sleep the night, go to the toilet one last time in the morning. Have a shower and head off for the procedure.
When your procedure is booked for the afternoon, the laxative timings adjust accordingly. I had to take one dose at 7pm the night before the procedure. I then had to get up at 6am and take the second dose, on the day of the procedure. As I’ll get on to, that can lead to some concerns.
Personally, I much prefer a morning slot for the procedure, thus getting both doses of laxatives over and done with the night before. I was tempted to do that this time, if only to avoid getting up at 6am! But I followed the instructions, like a good little patient.
In preparation for this post, I maintained a timeline of the effects of the doses of laxatives. It went a little something like this:
- Took the first dose at 7:30pm. Finished it at 8:30pm.
- In the hour that followed, my abdomen felt like it was getting tighter and tighter.
- 45 minutes after the dose, I started feeling cold. I actually had to put a long-sleeved undershirt on…
- 9:30pm, I spent an hour on the toilet. The egg based constipation made this far more uncomfortable than it needed to be. Next time, if I’m on a protein heavy low residue diet, I’ll take some gentle laxatives as I go.
- After about an hour, I took a break because my legs were going numb.
- 45 minutes later, I was back for another 20 minutes on the toilet. By this stage, what I was passing was effectively pure liquid.
- From midnight, I started feeling that I would need to go again before I could sleep. I decided to wait until I needed to go, to avoid getting up in the night.
- At 1am, I was back on the toilet for another 30 minutes.
- Shower!
- I got to sleep at gone 2:30am.
- Up again a 6am and drank the second dose over an hour.
- An hour later, I was on the toilet for 45 minutes.
- 9:45am and another 20 minute stint on the toilet.
- I was leaving for the hospital at 1pm, to make my appointment at 1:30pm, so I timed my last visit to fit around that. This turned out to be 30 minutes at around 12:15pm.
- Long, looooong shower.

Photo by John Fornander on Unsplash
This next bit is going to be too much information for some people. It’s useful to know but very specific. I’ll write it in blue. If you’re uncomfortable with details about bodily functions, avoid the text in blue.
When you’re on the toilet, your body is going to be telling you to ‘push’. Particularly if you have become a bit constipated. Resist this temptation hard. Believe me when I say that nature will take its course without you needing to push. If you do push, however, everything comes out much faster than it needs to. And this leads to splash-back. Just try and relax and let things move as slowly as you can. That said, make sure you have cleaning products on hand, just in case.
And then it’s off to the hospital to have your colonoscopy.
Once you arrive, there is still an element of paperwork to get through. You’ll be asked when you last ate and drank. You’ll also be asked a lot of the same questions you answered during your pre-assessment. Most importantly, you’ll be asked whether or not you want sedation. My response to the latter was, “Yes please…”
Unlike for a sigmoidoscopy, with a colonoscopy sedation is an option. The reason for this is that, while a sigmoidoscopy is minimally invasive, a colonoscopy is, presumably, ‘maximally’ invasive. It’s very likely that I’ve just made a phrase up, there. Regardless, because the colonoscope travels the entire length of the bowel, it is considerably more invasive.
Before that, though, you have to dress for the occasion. I was told to strip from the waist down, although I was allowed to keep on my socks. I then put on one of the those wonderful backless hospital gowns; at least this time there was good reason to be wandering around with my arse hanging out. When I was dressed appropriately, a butterfly cannula was put in the back of my left hand, ready to receive the sedative.
The reason that the sedative is offered is that, in order to travel the whole length of the bowel, it has to turn a couple of corners. If you refer back to the image at the top, you can see that these ‘corners’ have names: the left colic (splenic) flexure, and; the right coloc (hepatic) flexure. If I show you the image of the colonoscopy procedure from the Cancer Research UK site, I can explain how this differs from reality:
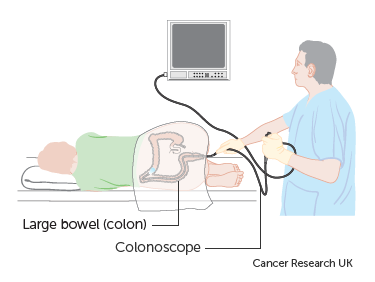
https://www.cancerresearchuk.org/about-cancer/cancer-in-general/tests/colonoscopy
Yeah, you see it doesn’t really work like that.
The colonoscope is too rigid to make such tight turns, which means that, to get all the way round, the corners (flexures) get smoothed out a bit. This can be uncomfortable, particularly during your first colonoscopy. For this reason, the sedative is offered. Gas and Air, or Entonox (nitrous oxide), is also on offer, either with the sedative or instead of the sedative. The sedative does make things easier but, as the NHS website explains, it comes with certain conditions:
“So if you have the sedative, it is important that you:
-
- don’t drive home
- avoid alcohol for 24 hours
- don’t make important decisions for 24 hours, and
- don’t operate machinery.“
I’ve managed to get all this mixed up with my colonoscopies. For my first one, I chose not to have a sedative, because I wanted to play hockey the following day. I found it pretty uncomfortable. Since then, I’ve gone with the sedative and they’ve both been simplicity itself. My suggestion would be to have the sedative the first time you’re having a colonoscopy. Thereafter, the Entonox should be fine. I might even listen to my own advice when my next colonoscopy is due.
There are a couple of other differences between your first colonoscopy, and any subsequent ones:
- While you start every colonoscopy by laying on your left side with your knees drawn up; during the first colonoscopy you’ll be asked to adjust your position. You may be asked to roll on to your back, and then back on to your side. This is so the operator can get the colonoscope around the corners. In subsequent colonoscopies, the corners have been smoothed out, so you’re unlikely to need to move your position; you can just lie back and think of England (other countries are available).
- During every colonoscopy, air will be pumped into your bowel to create the space the operator needs to see everything. The idea is that you relax enough to allow most of the air to escape during the course of the colonoscopy; so you don’t end up full of hot air. The problem is that during your first time, you try and fight this. This is to avoid spending the duration of the procedure endlessly farting on the operator. I mean, call me old fashioned, but that doesn’t seem right! After your first one, you simply don’t worry about this any more.
The actual process of having your colonoscopy begins after the sedation has been administered. Or the mask for the Entonox has been put in place. Or both. Of course, you can also choose to have neither. Whatever you choose, there will be a nurse there to talk to you and keep an eye on you. The nurses I’ve had during all my colonoscopies have been brilliant at making small talk, given the oddness of the situation.
The tip of the colonoscope, which has been thoroughly lubricated, is pushed inside you. It’ll be a bit on the cold side which won’t help the natural tendency to resist. But, as the Borg say; “resistance if futile!”

Marcin Wichary [CC BY 2.0 (https://creativecommons.org/licenses/by/2.0)]
After that, it’s just a case of chatting with the nurse while the operator introduces the 1,200 – 1,500mm (4-5 feet) length of the colonoscope into your body. If it’s uncomfortable, let the nurse know. This may well end up with you changing position but this might happen anyway. The operator will keep going until they get to the appendix or the junction with the small intestine. It’s likely that the operator will give you regular updates. You can also expect to be told if the operator has found something untoward and/or wants to take any biopsies.
And then it’s done. On the way out, the air pump will be reversed to withdraw as much air as possible. The operator will give you a quick wipe and then cover you up. From there you’ll be wheeled back to recovery, where you can rest until the sedative wears off, if you had any. When you’re ready, you’ll be invited to get dressed and the cannula will be removed, if you had one.
The last thing, before you can leave, is a chat about how it went. If there is something to discuss, this will be in a side room and you’ll be told what happens next. When I was taken off to a side room, it was to tell me that it looked like I had cancer and that I’d be sent off for some scans. When there’s nothing to discuss, I sit in a waiting room until a nurse judges I’ve had a long enough time to recover from the sedative. The nurse then tells me everything is fine and I’m allowed to go.
This, however, is not all that is involved in having a colonoscopy.
It takes at least a week for your body to get back to normal.
After having the colonoscopy, you’ll be famished and will probably eat immediately. Under normal circumstances, this will take two days to work through your body, so don’t expect regular trips to the bathroom for those couple of days. That said, it’s quite common to go within a couple of hours of getting home. The lining of your bowel can become a little irritated by the process of having a colonoscopy, which can result in a small amount of discharge. Don’t be worried if there’s some blood in this early visit, especially if any biopsies were taken.
If, on the other hand, you need to repeatedly go to the toilet and there’s always blood involved, call the aftercare number. You’ll be given a sheet with aftercare information, that will include a phone number for just this eventuality. Call it if you’re in any doubt.
And, by and large, that’s what’s involved with having a colonoscopy.
There is one other area that I want to mention but, again, it might be considered too much information. So, I’ve left it to the end to keep it out of the way. Again, I’ve written it in blue, so if you’re uncomfortable with details about bodily functions, avoid the text in blue.
When you arrive for your procedure, there can often be an element of waiting involved. If this waiting goes on long enough, you’re likely to find yourself maybe needing the toilet again. So now you’re faced with a quandary: you’ve had your shower, there’s no way to have another one. Is it better to make sure your bowel is empty, but undo the benefit of the shower? Or is it better to maintain external cleanliness but risk there being a puddle just inside?
As I explained, above, the colonoscope has a suction element that is activated immediately at the start of the procedure. And, knowing that, it then comes down to a judgement call. For my part, I recommend taking toilet wipes with you to the procedure. At least then you can do a good polish and shine, should you decide that going to the toilet is the best option.

I’m not saying this to be crude. Having a colonoscopy is an awkward situation. To my mind, anything that ensures it goes as smoothly as possible is good to know.

2 thoughts on “The Ins and Outs of Having a Colonoscopy – March Update”
I’ve been waiting for the outcome of your colonoscopy and it’s excellent news! So very happy for you and your loved ones
Thank you.