With the second recurrence of my bowel cancer, I was moved on to palliative care based around palliative chemotherapy. Coping with palliative chemotherapy turned out to be something of an adventure…
My first experience of chemotherapy had involved being rendered immobile for long periods of time by nausea. I was determined that this time would be different. That, while coping with palliative chemotherapy, I’d still get the most out of life. I’d exercise and maybe even lose weight. Determined, I was. Determined!
As it turned out, determination will only get you so far. Reality, however, will get you all the way up to 22 stone (140 kg, 308 lb)!
This seems like a good time to introduce you to the medications involved in coping with palliative chemotherapy:
FOLFIRI
The name FOLFIRI comes from the drugs involved:
- FOL – Folinic Acid
- F – Fluorouracil (5FU)
- IRI – Irinotecan
The folinic acid, also known as calcium folinate, isn’t actually a chemotherapy drug, it’s just a catalyst that makes the 5FU work better. I have no idea how someone discovered this…
Coping with palliative chemotherapy is all about the side effects. So, let’s have a look at some of those side effects, shall we…:
- Anaemia
- Bruising and bleeding
- Diarrhoea
- Eye problems
- Feeling sick
- Hair loss
- Skin changes
- Sore mouth
- Tiredness
I haven’t listed all the side effects; Ha Ha Ha, no! That would take up too much space. I’ve just listed the ones that affected me!
But, anyway; on to the other chemotherapy medication:
Cetuximab
Cetuximab is used to treat advanced cancer of the bowel and is a type of monoclonal antibody. It works by ‘targeting’ protein receptors on the surface of cells and can be referred to as a ‘targeted therapy’ as a result. It works by blocking the receptors that trigger cells to divide and grow, something that cancer cells do far too much of.
I was also told that its use was a one time deal. If I get to the stage where I need to be coping with palliative chemotherapy again, Cetuximab won’t be an option. A brief study of the side effects will help you decide whether this is a bad thing:
- Skin changes
- Tiredness
- Feeling sick
- Diarrhoea
- Sore mouth and nose
- Hair changes
- Nail changes
- Sore eyes
I’ve left these in the order they were listed, instead of going alphabetical, because I want to take a closer look at, Skin Changes:
‘You may develop an acne-like rash on the face, neck and body during the first three weeks of treatment. The skin may also become dry, itchy and flaky.’
Oh, I may develop acne, may I?! I may get itchy skin, huh?! Does this look ambiguous to you…!?

In an attempt to ward off some of the side effects of coping with palliative chemotherapy, I was given a whole bunch of other, non-chemotherapy, medications, including:
- Dexamethasone – A steroid to reduce the bloating
- Ondansetron – To combat the nausea
- Domperidone – To combat the nausea
- Loperamide – To combat the diarrhea
- Doxycycline – An antibiotic to combat the acne (six week course)
- Topical Hydrocortisone – Steroid cream to combat the acne
- Benzydamine Hydrochloride – Mouth wash to combat ulcers
- Prednisolone – Steroid eye drops to combat inflammation
In practical terms, taking these medications, while battling with chemo brain, required a system. Fortunately you can buy just about anything on Amazon…

So, all the medication was sorted. I knew what I was getting, the hospital knew what they were giving. I had my snazzy new PICC line nestling in the basilic vein of my right arm, so everyone knew how I was getting the medication. All that was needed was to go in and get it.
And, on March 14th 2016, exactly 22 years after I started my relationship with Julie, I also started coping with palliative chemotherapy. As with my previous chemotherapy treatments, I was administered at the specialist oncology day room at my local hospital. The Beacon Centre at Musgrove Park Hospital. And, as with my previous experience, the staff that looked after me were endlessly patient and caring. I remain enormously grateful for all that they do.
Getting a dose of chemotherapy starts with taking your seat in a room with four to six other people who are also receiving treatment. Because I had the PICC line, we were able to get going quite quickly. There was no need to find a vein and put in a cannula. Even so, the process lasted more than two hours
All the medications were administered by a ‘drip’. Although the drip is far more automated these days. The line from the bag of medicine is run through a machine that, essentially, pushes the chemo into you. The good thing about this process is that they set the rate and the time it takes, so you know how long you’ve got to snooze. And snooze is what I typically did. I played a recording of rain falling on a tent through some nice, comfy headphones and dozed the time away.
The cetuximab went in first, followed by the irinotecan. After that was a small dose of the 5FU (and, presumably, folinic acid). This was then flushed through, before the pump was attached. The ‘pump’ was a small plastic flying saucer shaped beast, full of extra 5FU. It lived in it’s own special handbag and had to stay in place for the full 48 hours that it would take to ‘pump’ this poison into me.
If you were wearing this pump in its handbag, and had a colostomy bag as well, you might look a little something like this:

This was not an easy thing to sleep with!
After the 48 hours were up, it was back to the hospital to get the pump disconnected. I then had to go back in, the following day, to get my PICC line cleaned. This was before Julie took over the PICC re-dressing duties, and this visit formed part of her training to do so. Anyway, while I was there, they decided I wasn’t acne-ridden enough and slipped in another dose of cetuximab. This was in addition to the mid-treatment dose of cetuximab that I was getting four days later. By the time my second treatment was due, three days after that, I had started referring to cetuximab as ‘Plague Giver’. I was not a pretty site.
I did keep my hair, though. This, believe it or not, actually came as something of a disappointment. You can see, in the photo above, that I had cut my hair short for the start of the chemotherapy, because I thought it was all going to fall out. I thought it would make less mess this way. Also, In my imagination, my hair loss was going to be like the Whomping Willow shedding its leaves in Harry Potter.
I could then get a ginger wig, in the style of a bob cut. My wife and daughters are ginger, to varying degrees, and I’ve made the occasional disparaging comment about this, over the years. I thought it would be right for them to get their own back. But I couldn’t. Because my hair didn’t fall out. It thinned for a while, but that was about it.
Because the treatments were in two week cycles, and there were 12 of them, they would run from March to September. This was right across holiday season and wasn’t fair on the girls. After a bit of negotiation, it turned out to be possible to slip a treatment back a week. And, in that way, we managed to sneak in a week in a cottage on the Isle of Wight, in June, and a week of camping in Perbrokeshire, in August.
I think that it’s important to try and fit in some family time, some memorable time, if you can. Not least because you never know what the next scan is going to show. Also, I was struggling with some of the side effects and an extra week off, here and there, allowed me to be more like myself around the girls.
Speaking of side effects, I’m doing to discuss some of mine. There will be photos…!
Let’s start with the nausea. It was bad and get progressively worse over the months and the courses of treatment. This meant that I spent a lot of time in bed and did very little exercise. Which is how I managed to climb up to 22 stone. Worse still was the percentage of this weight that was body fat. I don’t have figures, but I know I lost a lot of muscle mass because of how weak I felt when I started exercising again, after the chemo finished. Another, subtle hint, that I was too inactive and too flabby, was the development of Intertrigo. A sore that develops between ‘body folds’ or, in my case, rolls of fat.

On that note, you are given an… arm condom… to wear in the shower. It’s elasticated at either end to ensure a tight fit to the arm. This elasticated material, however, is not waterproof, meaning you have to keep it out of the shower as much as possible. Hence the need to try and shower one-handed as much as possible:

In terms of the skin and hair issues, which resulted both from the Plague Giver and the FOLFIRI, well, they ganged up and sent the acne into my scalp though the thinning hair. This resulted in apocalyptic levels of itchiness and some dramatic attempts to solve the problem.

Not satisfied with savaging the outside of my body, the Plague Giver started heading inland. In reality, it might not have just been the Plague Giver causing this, but I’m sure going to blame it. A concept seemingly reinforced by the notes from my meeting with the oncologist on 6th July:
‘He has a significant cetuximab rash and also ongoing mouth ulcers despite 2 dose reductions with the 5FU. In addition he has developed sore eyes.’
See! See!? If the 5FU had been reduced twice, it had to be the Plague Giver. As punishment for your skepticism, here’s a photo of the ulcers on my tongue.

In terms of the remaining things, I actually did okay from the diarrhea aspect. There were a couple of times things got more interesting than I’d have liked, remembering that I had a colostomy bag, but, by and large, I probably got off light. The only other notable side effect was the weirdness that happened to my nails…

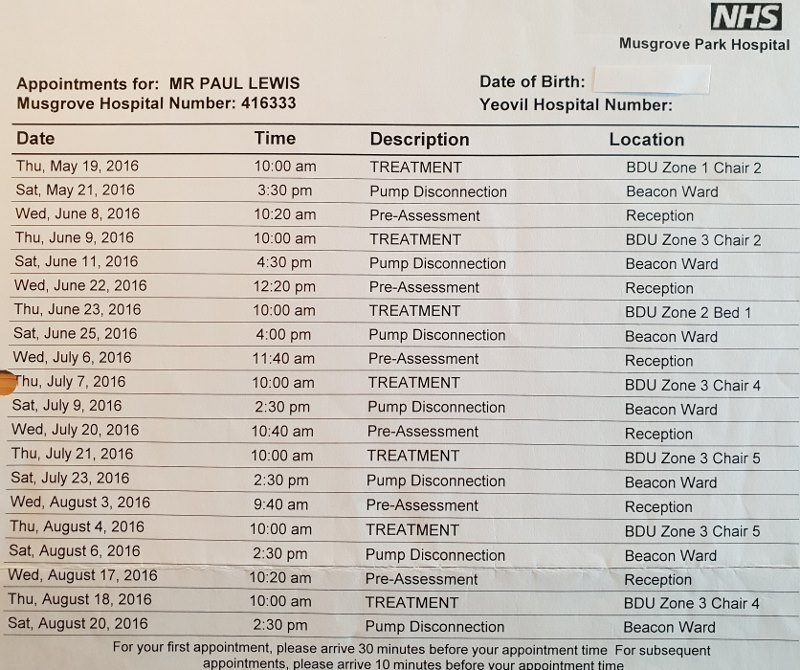
But coping with palliative care isn’t just about the symptoms, it involves a lot of trips to the hospital. That’s fine if you’re me; relatively young and fit. But if you have mobility issues and/or live a significant distance from the hospital, this will have to be taken into account and careful plans made. The list below gives an indication of the visits you will need to make. And this doesn’t include the additional trips that will be required if there’s no one at home to clean and dress your PICC line for you.
All in all, I found coping with palliative chemotherapy to be a dispiriting and uncomfortable affair. For me, coping with palliative chemotherapy was never actually terrible, it was just a long, drawn-out period of low-level.. misery. I was trying to think of the right word and was tempted to try and be more upbeat. But, the reality is, it was a miserable time. I was miserable!
But, it only went and worked…
I mean, I’m still here, writing this, more than two years later. I’ll take six months of low-level misery for that, any day of the week.
The very last part of this palliative chemotherapy fell on my 46th birthday, when I had the final pump disconnection. Of course, I still had the PICC line in, a colostomy bag, a head full of anti-depression medication and enough body fat to impress a walrus. There was work still to be done.
2 thoughts on “Coping with Palliative Chemotherapy”
Hello from Canada, it’s great to see that you haven’t lost your sense of humour.
Hi Linda,
It’s nice to know that someone thinks I’m occasionally funny.
All I get around here are tuts and eye rolls!
All the best,
Paul